Like No
Other
illustration by Ileana Soon

 n a normal day, Keren Osman ’92 works with stem cells as a bone marrow transplant physician at Mount Sinai Hospital in Manhattan.
n a normal day, Keren Osman ’92 works with stem cells as a bone marrow transplant physician at Mount Sinai Hospital in Manhattan.
When COVID-19 patients started appearing on the scene, much of the medical approach and focus was on the respiratory symptoms that accompany the disease. While these are proven to be a part of the impact from the coronavirus, physicians have since identified a host of other issues.
Osman is just one of hundreds of Swarthmore alumni helping to fight the disease. By bringing their expertise in health care, research, economic development, and mental health to those impacted by the coronavirus, alumni are making a difference in the current overwhelming climate of the pandemic.
“I had a conversation with one of my colleagues about a particular set of stem cells that were on the brink of approval for transplantation to treat a variety of illnesses,” Osman says. “We know that these cells help with inflammation and travel to the lungs first, so we wondered whether they might help with the inflammatory process we’re seeing in COVID patients.”
Osman and her colleagues quickly put together an application with the Food and Drug Administration for an emergency investigational new drug (EIND).
“This is a petition to try a therapy on a compassionate basis for patients with no other options,” she says. “In the early days of COVID, before any clinical trials, there were a good number of emergency INDs granted, including ours.”
After receiving FDA approval, Osman and her team tried the stem cells on their first patient and then quickly moved on to 12 more.
The first patient died from a pulmonary embolism, but Osman says the disease was likely too far advanced. “The next patient to receive the cells wasn’t as ill and did well,” she says. “We subsequently treated the others and successfully extubated nine and sent them home.”
Working from those encouraging results, Osman and her team petitioned the National Institutes of Health for funding of a larger study. “They agreed, so now we are opening a randomized clinical trial of 300 patients across 20 centers,” she says.
Osman is encouraged by the results of the early Sinai trial.
“The first 12 were very carefully chosen, so there may have been a selection bias,” she notes. “Could they have improved because of the cells? We don’t know, but no one got sicker and no one had an adverse reaction.”
As a physician on the front lines of the pandemic, Osman has a unique vantage point for how unprepared the country was for such a crisis.


There are only two surefire ways out of the pandemic: find a vaccine or acquire herd immunity, he says. The latter would require approximately 70% of the world’s population to be infected with the coronavirus, which would take years and leave hundreds of thousands of people dead in its wake. The viable solution, then, is a vaccine.
“The search for a vaccine is obviously ongoing and vigorous,” says Greenstone, the Milton Friedman Distinguished Service Professor in Economics at the University of Chicago. “But in the period until we get there, policymakers must make decisions about how to trade off economic and social activity with health risk based off very little information.”
It doesn’t have to be this way, says Greenstone. “Too often we rely on convenience samples — front-line workers, women arriving to give birth, or people with symptoms — and people who volunteer to take the test,” he says.
Instead, Greenstone suggests, by offering monetary incentives to a random subset of a representative sample, a greater portion of the population would willingly get tested. “Without monetary incentives, too many people decide that the benefits of getting a test are outweighed by the hassle — whether the swab itself, the cost, or the inconvenience.”
To test his theory on monetary incentives, Greenstone and some of his colleagues applied for and received a grant to test this idea in Chicago. “We’re rolling out invitations and randomly assigning the incentive,” he says. “The tests can be repeated regularly so that we can track how the disease is evolving and who is developing antibodies.”
The end goal, says Greenstone, is to understand the current prevalence of the disease in the population and use the results to guide reopening strategies. “Until we have a vaccine, knowing the population antibody rate is the name of the game,” he says.

A veteran public health official who has dealt with myriad disease epidemics — Ebola, SARS, the 2009 H1N1 influenza pandemic — Schuchat is well-skilled to serve in one of the nation’s very top positions addressing the COVID-19 pandemic.
That said, the coronavirus is like no adversary Schuchat has faced before.
“This is an extremely challenging virus,” she says. “Unlike others that have preceded it, this coronavirus can spread easily before symptoms show up, and even in cases where people are not symptomatic. It’s a stealth virus.”
Because of the sheer size of the outbreak, plus the virus’s tricky nature, the response is in a class of its own, says Schuchat. “The pandemic is not likely to end anytime soon, so the scale of response is unprecedented,” she says. “It doesn’t mean we’ll have a vaccine before the virus has made its way through the global community, but we’re doing all we can to scale up rapidly.”
That means cooperation between various nations and governments, and lots of funding directed at research.
“The work is going on concurrently rather than sequentially,” Schuchat says. “There’s a good deal happening at once, which is appropriate.”
As an undergrad in Swarthmore’s Honors Program, Schuchat majored in philosophy and biology, heading to Dartmouth for medical school upon graduation. She spent four years as a resident and chief resident in New York City, planning to be a clinician and internist — in the midst of the AIDS crisis. “After residency, I went to the CDC for the two-year Epidemic Intelligence Service program, and always assumed I’d move on from there,” she says, “but I discovered epidemiology and public health, and 30-plus years later I’m still here.”
Responding to the pandemic in her current role, Schuchat credits her liberal arts foundation at Swarthmore for arming her with the necessary skill set. “Having the ability to recognize different perspectives and the values that different communities bring to an issue is vital,” she says. “I can embrace complexity and recognize that action requires the best data and the right perspective. It’s quite valuable to me in this moment.” —A.L.

Growing up, Park, a novelist and creative writing professor at American University, spent many hours working in her parents’ grocery store in Brooklyn. As the pandemic began to roll across the country, she was hard at work on a second novel as a writer in residence at the Edith Wharton home in the Berkshires.
Park admits the shift has been difficult. “I haven’t worked here in a long time and never did it full time,” she says. “But I stepped into my father’s shoes and do a little bit of everything, from the cash register to packing bags and cleaning carts.”
— Patricia Park ’03
Here are but a few of the ways that Swarthmoreans looked out for the common good this spring and summer.
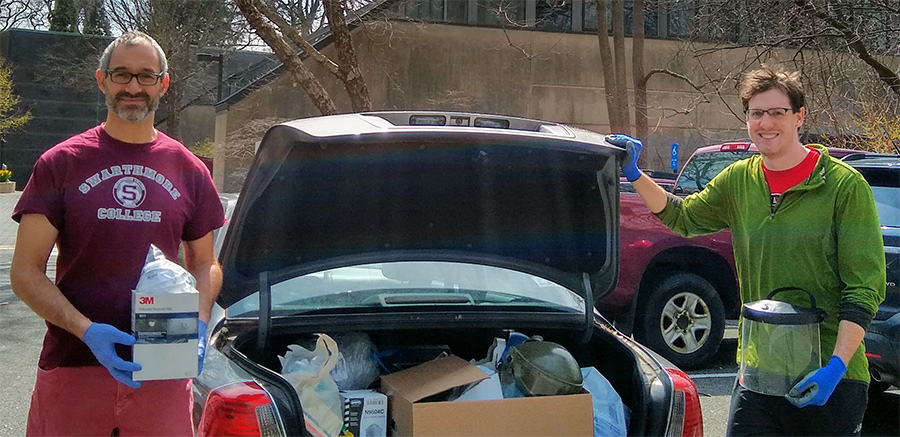
Supplies, in demand: Responding to requests for help from Penn Medicine hospitalist Farah Hussain ’09 and Temple University medical student Joe Corcoran ’16, faculty and staff members joined forces to gather personal protective equipment for Philadelphia medical professionals.
Nick Kaplinsky, associate professor and chair of biology, put out a call to his science and engineering peers, yielding three packed car loads of gloves, masks, Kevlar jumpsuits, goggles, disinfecting solutions, and more — supplies that went unused when classes turned virtual.
Meanwhile, the Environmental Health & Safety office gave away more than 500 N95 respirators from its long-held stockpile. And Greenhouse Manager Rhonda Hilt donated a self-contained respirator from her time at a nonprofit botanical garden.
“These donations are about hope,” Hilt says. “Our wish is that this small donation will show how much we appreciate and value the brave people doing this vital work for the greater good.”
Masks for all: LPAC Costume Shop Manager Tara Webb ’94 helped outfit the broader community this spring by organizing mask-making efforts to aid against the spread of COVID-19.
With volunteer help from about 30 faculty, staff, and students — including Chunyang Wang ’21, Rebecca Lin ’22, and Gwyneth Fletcher ’22 — Webb spearheaded a project to create a cache of masks for Swarthmore’s essential workers. Within days, the group had made 600 face coverings.
For Webb, organizing this effort served as “a little bit of a balm, because I’m doing something for other people,” she says. “I’m not a medical practitioner, but at least I can do this. That’s a good feeling.”
Shelter and sustenance: For years, Rod ’67 and Dorothy Woods Chronister ’66 have joined their church in preparing lunches for those in need of a meal. But when the pandemic hit in early March, the volunteers realized adjustments were needed to keep bellies full and participants safe.
To aid in physical distancing, the group moved from the church’s building to a nearby park, offering community members a “grab-and-go” meal of a brown bag, fruit, and a beverage. Guests were encouraged to maintain 6 feet of separation, while volunteers diligently disinfected tables and supplies.
“Other programs have had to cut back in providing meals,” says Rod, a retired physician. “Now, with the pandemic, there are even fewer options” for those in need.
Isaac Stanley ’73 had a similar concern as board chair of Ignite, a Chicago-based agency that provides support for youths on the brink of homelessness. Although volunteer efforts had to be halted temporarily, Ignite remained fully staffed, with overtime and hazard pay instituted to ensure the agency could keep running.
The additional costs, however, came just as the agency was forced to cancel its biggest annual fundraiser. So Stanley and the board got creative — pivoting toward a virtual celebration that brought in $337,000 to help keep youths housed and fed.
“One of the things I’ve learned from this whole experience … is the role of philanthropy,” Stanley says. “Everyone who’s part of the College is very aware that if you have the means to give back, it’s your duty to take care of those who are in need.”
Park’s Swarthmore education helped instill in her a sense of community, she says. “Working in a grocery store, it’s hard to give personalized attention to every customer, but I’ve found little pockets of connection. I look for the humanity in the midst of the pandemic.”
Before the pandemic hit, Orr Harmeling provided her care to patients and staff in both the acute care and psychiatric wings. When COVID arrived, her team split into remote and in-person caregivers, with Orr Harmeling taking up a remote role.
“I am calling patients, families of patients, families of the deceased, and also providing phone and Zoom support to our staff,” she says. “The pandemic is especially hard on people because it removes human connection at a time when it is most needed.”
Orr Harmeling has become creative in her care with COVID patients and families: “I ask family members to write a bio of their loved one, and then caregivers place it above their beds,” she says. “We also ask for any messages from the families to their loved ones and the staff. It personalizes the patients for the medical staff and lets the patients know their loved ones are thinking of them. The staff will convey messages and jokes to the patients — whatever will lift their spirits and give them a will to live.”
Orr Harmeling also frequently uses French, Spanish, and German in her work and credits her preparation at Swarthmore for those skills.


Harris Stanley tends to a high-risk population in Chicago, made up of older patients and the chronically ill. As She made the quick pivot to telehealth when the pandemic began. “We need to protect our staff and the people we serve,” she says. “We want to ensure that no one gets sick because of us.”

Co-authored with Philip Gressman, a mathematics professor at the University of Pennsylvania (and also Peck’s husband), “Simulating COVID-19 in a University Environment” projects how the coronavirus could spread across campuses and the steps schools can take to minimize its impact.
Basing their study on a campus the size of Penn, with 20,000 students and 2,500 faculty members, Peck and Gressman found that a combination of simple interventions could limit infections to about 50 over 100 days, with only about 200 people quarantined at any given time.
“It surprised me how well these strategies all work all together,” says Peck. “This is consistent with what we’ve observed in the larger spread of the disease, but if people are social distancing, mask-wearing, and not meeting in large groups, all these things together can keep the reproduction of the disease pretty low.” — Elizabeth Slocum
— Ava Harris Stanley ’72
Despite the change in her health care delivery approach, Harris Stanley says it serves as a silver lining. “It facilitates clinical medicine when a patient can’t get to you for a host of reasons,” she says. “Fragility, distance, and other factors can make getting to the office difficult. We wouldn’t have arrived at this point were it not for the pandemic.”
As with other health care providers, Harris Stanley has recognized the need for self-care throughout the crisis. “My husband has developed phone meditations that he facilitates,” she says. “I’ve returned to birding, and we’ve gone on many more walks.”
This self-care has become especially important to Harris Stanley as a Black woman and mother to two sons. “This has been a double epidemic, one exposed by cellphones,” she says. “I had to teach my sons at a very young age to protect themselves, and now the world sees why. It’s painful to me.”
“It was an incredibly rapidly evolving situation,” says Vedanthan, associate professor in NYU Langone’s Departments of Population Health and Medicine. “I fundamentally felt like it was the right thing to do to volunteer.”
The risks were real. After discussing the commitment with his wife, Board of Managers member Sujatha Srinivasan ’01, Vedanthan says as a family they mentally prepared as much as possible. “As long as the institution would do what it could to provide me with protection,” he says, “I would try to minimize the chance of falling ill by doing everything I could, like washing my hands, wearing double gloves, face shields, and all the PPE provided.”

“There was a lot of learning on the fly — but not chaos,” he says about the 7 a.m.-to-7 p.m. shifts. “All of my patients were either confirmed COVID-positive or suspected COVID.”
The experience was emotionally and mentally draining. His time on the wards, and then a two-week quarantine, meant he was apart from Srinivasan and their two young children for five weeks.
“Every day I was there, I was hoping I wouldn’t fall sick,” he says. “It’s given me a sense that it’s important to not take small moments for granted, like time with family and friends.”
As Vedanthan reflects on the past five months, his perspectives on the pandemic have evolved.
Through the lens of a physician, Vedanthan is stunned by the efficiency of the deadly virus. “Just how amazingly, incredibly powerful and devastating the COVID infection could be to a person,” he says. He witnessed as it “attacked every organ system you could think of. It’s remarkable to see the devastation it could do to a body — a biological ravaging. It’s very silent in the way it is transmitted, but I would say unprecedented in terms of protean and varied clinical manifestations.”


“Tech thinks it can solve all the problems in the world, and it can’t,” Ferguson, a software engineer, told The Philadelphia Citizen. “But this was a place where actually it can. This was like the winner case where, really, the need is technology.”
Many others have since joined those four, and Tsui has become something of a guardian angel to them. A student enrolled in the nurse practitioner program at Columbia University, Tsui felt compelled to go to work with COVID patients. Because Tsui is immunocompromised, his doctor told him not to work in the ER or ICU. “I found work at a nursing home,” he says.
— Justin Tsui ’05
Tsui can see his efforts being needed easily until the end of the year, noting that the government’s response to the virus hasn’t been sufficient.
“I’m worried,” he says, “but hopeful that more people will come out and vote and that we will get change.”
I first met Nick at a pre-orientation party for members of his class in New Jersey, and we became fast friends. We worked together on the Phoenix and shared a quad in Wharton my senior year. We spent much of our 20s living in group houses together in Washington, D.C. When Nick moved to New York in 1999, I knew it was time to grow up. I got married, and Nick took up marathon running, which took him to all seven continents. That kind of dedication and commitment was a hallmark of Nick’s life. He never did anything halfway.
Following his death, articles about Nick ran in People magazine, the New York Post, and Runner’s World.
In a segment on CNN, Anderson Cooper marveled that Nick had run marathons all around the world. “What an incredible life he led,” Cooper said, adding, “I wish I had met him.”
Meanwhile, Nick was one of the “remarkable people” that CBS This Morning featured in a segment titled “Faces of the Pandemic.”
Those of us who loved Nick know that he would have been as surprised as anyone by his sudden fame. A journalist for the Associated Press for nearly three decades, Nick was as humble as they came. He was far more comfortable writing about others than himself. In these very pages, as a class secretary, Nick chronicled the lives and accomplishments of his classmates for decades.
Anderson Cooper was right. Nick lived an incredible life, even if it was cut way too short.

It’s an important effort when it comes to helping developing countries manage the pandemic. As soon as the disease began spreading, Anderson and his colleagues started considering how to best support dozens of governments in their COVID-19 response efforts. “With the exception of developed economies, we can give support to just about any country,” Anderson says. “We’ve given support to over 100 countries so far.”
The World Bank established a fast-track financing facility and allocated billions of extra dollars in support of developing countries. “We looked at our internal policies to speed up preparation, review, and approval of projects,” Anderson says. “Normally, projects require six to 12 months for approval. We figured out which steps we could skip to expedite funding.”
Once released, the funding helped the countries increase ICU capacity, purchase PPE, and respond to other emergency needs. The next phase of Anderson’s work will involve the socioeconomic response the countries will need, he says. When he compares the pandemic to other crises he’s addressed during his time with the World Bank, Anderson says he hopes it is “a once-in-a-career event.” His Swarthmore education well-equipped him with the critical thinking and problem-solving skills he needs for his job.
“Those are the most useful skills I have to respond in a situation like this,” he says. “It’s been a privilege to be part of a team that can make a bit of a contribution to a massive effort like this.”